In the rapidly evolving world of regenerative medicine and performance optimization, healing and repair peptides have emerged as powerful tools for accelerating recovery and promoting tissue regeneration. These specialized protein fragments are revolutionizing how we approach injury recovery, wound healing, and overall cellular repair processes.
Understanding Healing and Repair Peptides
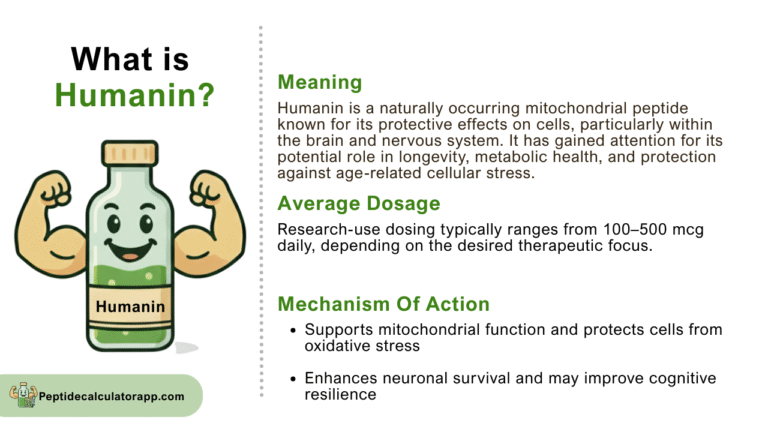
Peptides are short chains of amino acids that serve as signaling molecules in the body, directing various biological processes including tissue repair, inflammation reduction, and cellular regeneration. Unlike traditional medications that often mask symptoms, healing peptides work at the cellular level to promote natural recovery mechanisms and enhance the body’s inherent ability to heal itself.
These bioactive compounds function by binding to specific receptors on target cells, triggering cascades of beneficial biological responses. From stimulating collagen production to enhancing blood flow and reducing oxidative stress, repair peptides offer a multifaceted approach to accelerated healing that addresses the root causes of tissue damage and dysfunction.
Key Peptides for Accelerated Recovery
BPC-157: The Body Protection Compound
Body Protection Compound-157 stands as one of the most researched and effective healing peptides available. Originally derived from human gastric juice, BPC-157 demonstrates remarkable ability to accelerate healing of various tissue types including tendons, ligaments, muscles, and even neural tissue. This peptide promotes angiogenesis (formation of new blood vessels), which is crucial for delivering nutrients and oxygen to damaged areas.
Clinical studies have shown BPC-157’s effectiveness in treating tendon injuries, muscle tears, and even gastrointestinal disorders. Its unique mechanism involves stabilizing cellular structures and promoting the expression of growth factors that are essential for tissue regeneration.
TB-500: Thymosin Beta-4 Fragment
TB-500, a synthetic version of thymosin beta-4, plays a crucial role in wound healing and tissue repair. This peptide is particularly effective for soft tissue injuries and has shown promising results in treating muscle strains, ligament damage, and chronic injuries that have been slow to heal through conventional methods.
The peptide works by promoting cell migration, which allows damaged tissues to recruit healthy cells for repair. Additionally, TB-500 helps reduce inflammation while simultaneously encouraging the formation of new blood vessels and muscle fibers.
IGF-1 LR3: Enhanced Growth Factor
Insulin-like Growth Factor-1 Long R3 represents a modified version of natural IGF-1 with enhanced stability and potency. This peptide excels at promoting muscle growth, improving recovery times, and enhancing overall tissue regeneration. IGF-1 LR3 stimulates protein synthesis and helps maintain muscle mass during periods of injury or reduced activity.
Mechanisms of Action in Tissue Repair
The effectiveness of healing peptides stems from their ability to influence multiple pathways simultaneously. These compounds enhance cellular communication, optimize nutrient delivery, and coordinate the complex process of tissue regeneration. Key mechanisms include:
- Angiogenesis stimulation: Promoting the formation of new blood vessels to improve circulation and nutrient delivery to damaged tissues
- Collagen synthesis enhancement: Accelerating the production of structural proteins essential for tissue strength and integrity
- Anti-inflammatory effects: Reducing chronic inflammation that can impede the healing process
- Cellular proliferation: Encouraging the division and multiplication of healthy cells to replace damaged tissue
- Antioxidant activity: Protecting cells from oxidative stress that can delay recovery
Applications in Sports Medicine and Recovery
Athletes and fitness enthusiasts are increasingly turning to healing peptides to overcome injuries and enhance recovery between training sessions. These compounds offer several advantages over traditional recovery methods, including faster healing times, reduced risk of re-injury, and improved overall tissue quality.
Common applications in sports medicine include treatment of acute injuries such as muscle strains and ligament sprains, management of chronic conditions like tendinitis, acceleration of post-surgical recovery, and prevention of overuse injuries in high-performance athletes.
Chronic Injury Management
For individuals dealing with persistent injuries that have failed to respond to conventional treatments, healing peptides offer new hope. These compounds can help break the cycle of chronic inflammation and poor healing that characterizes many long-standing injuries. By addressing the underlying cellular dysfunction, peptides can restart stalled healing processes and promote complete tissue regeneration.
Administration Methods and Protocols
Healing peptides can be administered through various routes, each offering distinct advantages depending on the specific condition being treated and the peptide being used. Common administration methods include subcutaneous injection, which provides systemic effects and is suitable for most healing peptides, intramuscular injection for localized treatment of specific muscle groups, and topical application for certain peptides targeting skin and superficial tissue repair.
Proper dosing protocols are essential for achieving optimal results while minimizing potential side effects. Most healing peptides are administered in cycles, with treatment periods followed by rest phases to prevent receptor desensitization and maintain effectiveness over time.
Safety Considerations and Side Effects
While healing peptides are generally well-tolerated, proper medical supervision is essential for safe and effective use. Most side effects are mild and transient, potentially including temporary redness or irritation at injection sites, mild fatigue during initial treatment phases, and occasional headaches as the body adjusts to treatment.
Contraindications may exist for individuals with certain medical conditions, including active cancer, severe kidney or liver disease, and pregnancy or breastfeeding. Comprehensive medical evaluation and ongoing monitoring are recommended for all peptide therapy patients.
Future Directions in Peptide Therapy
The field of healing and repair peptides continues to evolve rapidly, with new compounds and applications being discovered regularly. Emerging research focuses on combination therapies that utilize multiple peptides synergistically, development of more stable and potent peptide formulations, investigation of oral delivery methods to improve patient compliance, and exploration of peptides for specific conditions such as neurological injuries and age-related tissue degeneration.
Optimizing Peptide Therapy Results
To maximize the benefits of healing peptides, patients should maintain proper nutrition to support tissue repair processes, engage in appropriate physical therapy and rehabilitation exercises, ensure adequate sleep for optimal recovery, manage stress levels that can interfere with healing, and follow prescribed treatment protocols consistently.
The integration of healing peptides with comprehensive recovery programs often yields superior results compared to peptide therapy alone. This holistic approach addresses all aspects of the healing process and creates an optimal environment for tissue regeneration.
As our understanding of peptide biology continues to advance, these remarkable compounds are poised to play an increasingly important role in regenerative medicine and recovery optimization. For individuals seeking to accelerate healing, overcome chronic injuries, or enhance their body’s natural repair mechanisms, healing and repair peptides represent a promising frontier in modern healthcare that offers hope for faster, more complete recovery from a wide range of conditions.